Onyx wins Best in KLAS.

OnyxEPA allows payers to determine whether prior auth is necessary and identify the test results and documentation required to support the request – all in real time.
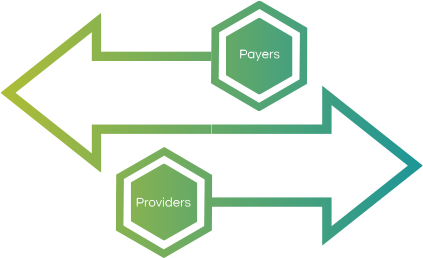
OnyxEPA supports bidirectional information exchange between providers and payers, works with all payer systems, and meets all HL7 FHIR standards.
Integrates payer queries into your EMR/EHR system
Employs clinical query language and FHIR questionnaires to define payer requirements for authorization and automatically extracts information from your EMR/EHR system
Bundles required documentation and submits to the payer for immediate determination or flagging for further review